This Week In COVID-19 Research: 3
Mikolaj Poplawski examines the latest papers including three leading COVID-19 vaccine possibilities, hydroxychloroquine claims, and the way in which SARS-CoV-2 tricks the immune system.

For Cambridge students, the most important news event this week was the University‘s decision to move next year‘s lectures online and the media furore this entailed. Meanwhile, in COVID-19 science, the leitmotiv of the week was vaccine development: obviously, creating and producing an effective vaccine against COVID-19 is of utmost importance. So far, however, the speed record of 5 years for a new vaccine belongs to the Ebolavirus rVSV-ZEBOV vaccine. Whether scientists can beat this now remains to be seen.
Phase I trial of Moderna‘s mRNA-1273 vaccine candidate
mRNA vaccines are a novel technology that potentially offer more scalability and could greatly simplify repurposing existing vaccines for emerging diseases. However, no mRNA vaccine has been approved for human usage, with several of them failing trials for side effects.
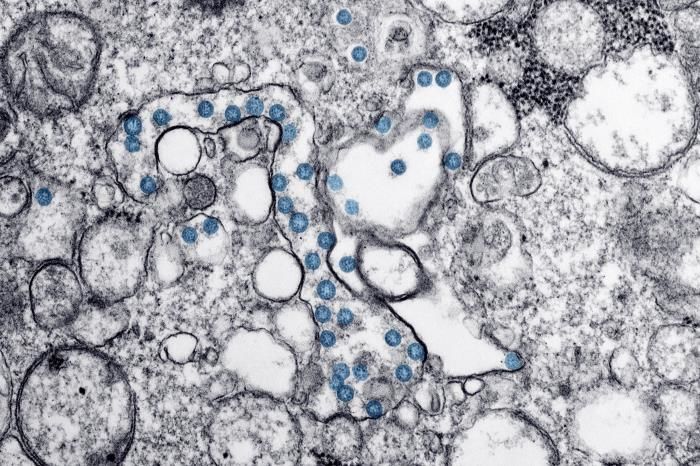
Moderna’s vaccine delivers a sequence of chemically modified mRNA molecules to get the body’s cells to produce the spike protein of SARS-CoV-2. The mRNA is contained in liquid nanoparticles (LNPs) that Moderna had developed as vectors for other mRNA vaccines. On Monday (18th May) Moderna announced the results of the first human trial of the vaccine. Phase 1 trials serve to ascertain the safety of a drug and to decide on the dose for subsequent trials. So far, the results look encouraging, although no one knows how good the antibodies raised by the vaccine are at preventing the development of the disease. The cohort that received a 25 µg dose had blood antibody levels comparable to people who have recovered from the disease. Higher doses (100 and 250 µg) produced even higher antibody levels, but the 250 µg dose was found not to offer many additional benefits while causing more significant side effects. Based on these results, a Phase II trial that should commence soon has been amended to use two doses – 50 µg and 100 µg.
A review of mRNA vaccines here.
Moderna’s press release here.
ChAdOx1 nCoV-19: the vaccine candidate from Oxford
Last week, we reported on the results of animal trials of a SinoVac-made inactivated virus vaccine candidate. Both Oxford and SinoVac trialed their vaccines in rhesus macaques. Unlike SinoVac, the Oxford team recovered virus RNA from all of their test animals. Does it mean that Oxford’s vaccine is ineffective? The test conditions were too different for us to learn anything by comparing the data. Oxford used twice as much SARS-CoV-2 to infect their animals, they also did not limit themselves to the upper respiratory tract and delivered the virus to the lower respiratory tract too. The amount of viral RNA in nasal swabs was unchanged in all groups, but vaccinated macaques had less of the virus in their bronchoalveolar lavage (BAL) fluid and their respiratory tract. None of them developed pneumonia, unlike 2/3 of the control group. It is unclear whether the vaccine protects the upper respiratory tract better at more realistic exposure to the virus. A Phase I trial with more than 1000 human volunteers is underway and recruitment for Phase II/III trials has begun.
Paper here.
“All treatment groups [with hydroxychloroquine] were found to have an increased mortality”
Harvard’s DNA vaccine candidate – another rhesus macaque study
Like Moderna, Harvard also opted for a nucleic acid vaccine, though they used DNA rather than mRNA. DNA vaccines are also a relatively novel technology and also have no approved human vaccines, but a few are used in animals. Like in Oxford, the test animals had SARS-CoV-2 delivered both by the intranasal and by the intratracheal route. Two of Harvard’s test vaccine formulations significantly reduced the viral load detected both by nasal swab and in the bronchoalveolar lavage (BAL) fluid. As in Oxford, the vaccines were better at decreasing viral load in BAL. This was especially true for the weaker formulations which cause only little or no decrease in viral load in nasal mucus. They also found a correlation between the concentration of neutralising antibodies in BAL and to a lesser degree (possibly due to the variability of nasal swabs) in nasal mucus. This is good news because if this correlation holds in other studies, we have a simple way of measuring the effectiveness of vaccine candidates.
Paper here.
Hydroxychloroquine meta-analyses
The most publicised attempt at drug repurposing against COVID-19 uses hydroxychloroquine (HCQ). Many trial results have been published, many of them quite flawed. To try and get over their limitations, a number of meta-analyses have been conducted. One of them was uploaded to medRxiv on Sunday 17th, one of them Wednesday 20th. Neither of them has found better recovery in patients taking HCQ, and both of them found increased side effects commonly associated with HCQ.
On Friday, an additional meta-analysis was published by The Lancet that looked at data from all around the world regarding the effectiveness of combinations of HCQ or chloroquine (CQ) with macrolide antibiotics. All treatment groups were found to have an increased mortality compared to the control group. Two months ago, when it was proposed that HCQ may slow down SARS-CoV-2 replication by affecting cellular vesicles, the side effect that was feared the most was disrupting the heart’s rhythm (QT Interval prolongation). Sadly, this risk has just been confirmed, with all groups receiving HCQ or CQ being at a higher risk of developing de-novo ventricular arrhythmia. An interesting thing to note about this study is that the authors also found that a group of drugs called ACE inhibitors decrease the risk of death, corroborating earlier reports, including some of the retrospective reports from Hubei.
Sundays’s paper here.
Wednesday’s paper here.
Friday’s paper here.
SARS-CoV-2 tricks the immune system in a unique way
COVID-19 patients respond unusually to viral infection. Normally, upon viral infection, there will be an elevated production of proteins that send a message to other cells to strengthen their antiviral defence. There are two arms of this response:
- one initiated by Interferon Regulator Factors (IRFs) that cause the infected cell to produce Interferons I and III, among other things
- one initiated by Nuclear Factor κB that leads to the production of chemokines and Interleukin 6
Various viruses have their own ways of preventing cells from signalling infection, but SARS-CoV-2 does it in a ‘distinct’ way. SARS-CoV-1 and MERS also attempt to downregulate the first arms of cellular defence, but SARS-CoV-2 is more successful at blocking Interferon production. Such abnormal, unbalanced response often leads to a very dangerous inflammation in the lungs. Therefore, decreasing the degree of inflammation by blocking the action of Interleukin 6 may be beneficial for patients with COVID-19. A Cambridge-led trial is being conducted to test whether approved anti-inflammatory drugs that target elements of the Nuclear Factor κB pathway result in better outcomes for COVID-19 patients.
Original paper here.
University’s article here.
 News / Pembroke to convert listed office building into accom9 December 2025
News / Pembroke to convert listed office building into accom9 December 2025 News / Gov declares £31m bus investment for Cambridge8 December 2025
News / Gov declares £31m bus investment for Cambridge8 December 2025 Features / Searching for community in queer Cambridge10 December 2025
Features / Searching for community in queer Cambridge10 December 2025 News / Uni redundancy consultation ‘falls short of legal duties’, unions say6 December 2025
News / Uni redundancy consultation ‘falls short of legal duties’, unions say6 December 2025 Lifestyle / Into the groove, out of the club9 December 2025
Lifestyle / Into the groove, out of the club9 December 2025