The battle against antimicrobial resistance
Elizabeth Zachariah puts our strategies for dealing with superbugs under the microscope
The threat of antimicrobial resistance (AMR) is immense, and has the potential to take modern medical practice back to the ‘dark ages’ - highlighted 10 years ago by then prime minister David Cameron. AMR is not a brand new challenge facing politicians, policy makers, and healthcare workers. Instead, many scientists would describe it as an insidious threat that is ever growing against a backdrop of disordered global affairs.
What is antimicrobial resistance?
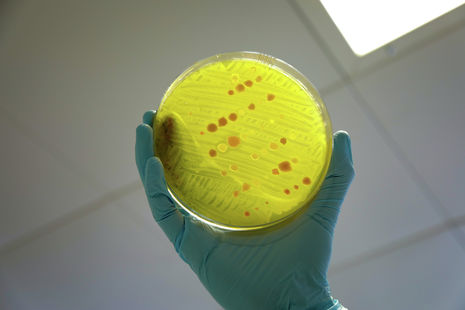
You may already be familiar with Charles Darwin’s theory of evolution. AMR arises due to evolutionary adaptation. The use of antimicrobial agents instigates an arms race with the pathogen (the bacteria, virus, fungi or parasite) that is being targeted. Whereupon a small number of pathogens within the infection acquire a mutation, this allows them to evade the effects of the antimicrobial drug being used. This leads to the expansion of a resistant subpopulation, precipitating an AMR infection. As a result we are now facing the emergence of ‘superbugs’ that are resistant to existing antimicrobial agents.
Although AMR can refer to drug resistant bacteria, viruses, fungi, or parasites, antibiotic resistant bacteria seem to pose the greatest threat to humanity. It is estimated that bacterial AMR contributed to 4.95 million deaths in 2019. Therefore the consequences of antibiotic resistance are not merely a supposed future but a grim reality. Bacterial AMR affects both those who contract bacterial infections but also patients who are being treated for other conditions. This is due to the reliance of modern medicine on the use of preventative or ‘prophylactic’ antibiotics. Any patient requiring surgery or chemotherapy will require antibiotics to reduce infection risk. In addition to the threat posed by antibiotic resistant bacteria, patients affected by non-bacterial infections such as malaria are also at an increasing danger of developing untreatable infections. In the 1980s, a wave of resistance to chloroquine (the drug of choice for malaria at the time) swept across the African continent, killing millions and making this treatment obsolete. Alarmingly, it’s possible this could happen again: resistance to artemisinin, upon which antimalarial treatment currently depends, has been recorded in multiple locations across Africa in recent years.
“Although AMR can refer to drug resistant bacteria, viruses, fungi, or parasites, antibiotic resistant bacteria seem to pose the greatest threat to humanity”
AMR can be considered an inevitability, but is there anything that can be done to slow down the emergence of drug resistant microbes? Antimicrobial stewardship refers to optimisation of the use of antimicrobials through careful drug choice, dosage, route and duration of administration. Healthcare providers can apply antimicrobial stewardship to daily practice in an effort to slow emergence of AMR. For instance doctors should reduce unnecessary prescription of antimicrobials, for example by avoiding prescribing antibacterial drugs for a viral chest infection.
AMR can also be fuelled by factors external to the hospital. Use of antimicrobials in livestock farming is known to further drive AMR. Furthermore, environments lacking adequate sanitation, hygiene, and access to clean water in conjunction with poor infection prevention measures facilitate the development of AMR. This is illustrated by a report published by Swedish researchers at the Lund University who found ‘extensive antibiotic resistance observed in gram-negative bacteria isolated from injured hospitalised war victims with nosocomial infections in Ukraine’. The report highlighted the involvement of inadequate infection prevention and control in the development of AMR in Ukrainian hospitals due to immense pressures as a result of limited resources due to the war in Ukraine.
“Developing countries may lack the critical investment needed to implement effective AMR action plans”
What is being done to tackle AMR?
Recent development of national and international policy to combat the rising tide of AMR offers hope in providing a unified front against the threat of ‘superbugs’. A key deficiency, highlighted by the World Health Organisation (WHO), in global action against AMR is the lack of ‘sustainable financing to implement activities in all sectors’. Many nations do not allocate sufficient financial resources to effectively implement the ‘national action plans’ outlined by the WHO. Within the UK, a 5 year plan to combat antimicrobial resistance was published this year. The plan sets out the need for strengthened monitoring and surveillance of AMR. The implementation of AMR-related policy within the UK already shows promise, as sales of antibiotics for use in food-producing animals have fallen by nearly 10% in the last year and more than halved since 2014. However, the extensive action plan introduced in the UK is unlikely to be mirrored uniformly across the globe. Developing countries may lack the critical investment needed to implement effective AMR action plans. In 2022, the UK invested £210 million to partner with countries across Asia and Africa to tackle AMR, but it remains to be seen whether such foreign aid agreements will rectify fragile AMR action plans in developing countries or whether it will only serve to paper over the cracks.
“Large pharmaceutical firms often view antimicrobial drug development as less profitable”
Development of new antimicrobials and novel therapeutics
Running out of suitable antimicrobial agents for treating drug resistant infections is becoming an increasingly common occurrence. Pharmaceutical companies therefore can play a key role in developing novel antimicrobials to treat drug resistant infections. However, many criticise Big Pharma for abandoning antimicrobial drug development. Large pharmaceutical firms often view antimicrobial drug development as less profitable when compared to other therapeutic opportunities such as cancer treatments. This is due to a combination of the low sale price and volume sold of most antimicrobials, as well as concerns doctors may avoid prescribing antibiotics due to fears of AMR. Additionally, the short treatment cycle for antibiotics contrasts against therapies for chronic diseases, which can be taken for many months, offering a more secure and long-term form of revenue for pharmaceutical companies. Governments can address this pipeline problem by implementing creative policies to support antibiotic drug development. For example the UK (in its 5 year plan) has committed to a world-first ‘subscription model’ for antimicrobials which incentivises the pharmaceutical industry to back antimicrobial drug development through paying the companies ‘a fixed annual fee for antimicrobials based primarily on their value to the NHS, as opposed to the volumes used’.
Furthermore, advances in biomedical science have spearheaded research into possible non-traditional antimicrobial agents; utilising biologics such as bacteriophages, antibodies, anti-virulence agents, and immune-modulating agents. Emerging technologies of the 21st century paving the way for a ‘fourth industrial revolution’ also offer new opportunities for innovation within the field of antimicrobial drug development. Artificial intelligence, for example, is becoming increasingly used within the context of biomedical research. Recently researchers collaborating across McMaster and Stanford universities developed a generative AI model, SyntheMol, that could design easy-to-synthesise antibiotic compounds utilising already-established reactant molecules and synthesis reaction pathways.
The challenges posed by AMR require the mitigation of both biological and organisational challenges through international collaboration. Fighting AMR is ultimately reliant upon introduction of policy which is effectively implemented. While the newly incumbent labour government has committed to fixing public services, it cannot afford to neglect the existential threats, such as AMR, facing humanity as we advance through the 21st century.
 News / Hundreds of Cambridge academics demand vote on fate of vet course20 February 2026
News / Hundreds of Cambridge academics demand vote on fate of vet course20 February 2026 News / Judge Business School advisor resigns over Epstein and Andrew links18 February 2026
News / Judge Business School advisor resigns over Epstein and Andrew links18 February 2026 News / University Council rescinds University Centre membership20 February 2026
News / University Council rescinds University Centre membership20 February 2026 News / Petition demands University reverse decision on vegan menu20 February 2026
News / Petition demands University reverse decision on vegan menu20 February 2026 News / Caius students fail to pass Pride flag proposal20 February 2026
News / Caius students fail to pass Pride flag proposal20 February 2026